
OR
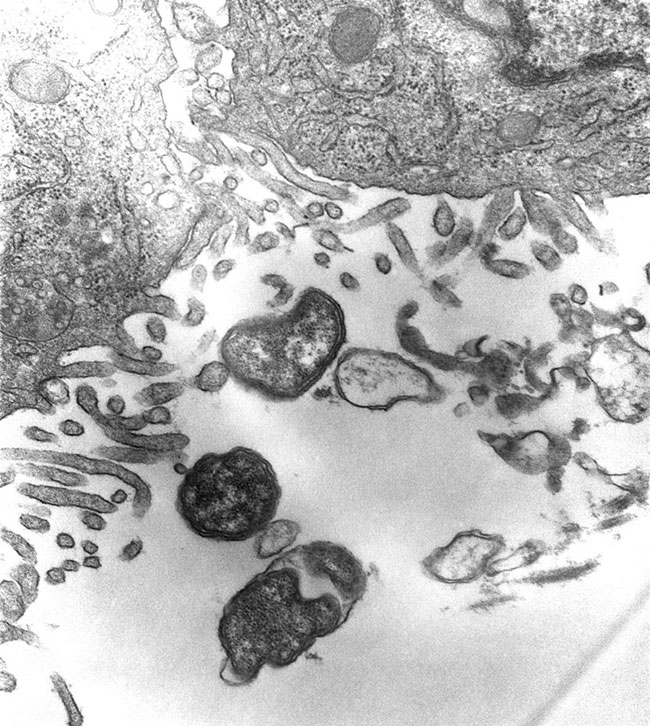
City dwellers may not know that Scrub typhus has been making a shift from rural to urban areas
Until August 20th, at least 22 Scrub typhus cases were diagnosed among patients with fever who visited the out-patient department of Sukraraj Tropical and Infectious Disease Hospital as well as among those referred there from various hospitals of Kathmandu. Many patients who were positive for Scrub typhus had no history of travel beyond Kathmandu city. For the first time, I have observed an unexpected number of Scrub typhus cases in a relatively short time in Kathmandu, the largest urban center in Nepal. In other words, there has been an outbreak of Scrub typhus in Kathmandu.
Until recently, the majority of Scrub typhus cases were reported from remote rural areas. As Scrub typhus is more common in the rainy season, we can expect more cases in the days ahead.
In Nepal, usually, health care workers do not try to identify the cause of fever and view any fever as typhoid fever. Patients thus at first receive medicine for typhoid from health care workers or they self-medicate, which is common in Nepal. By late identification can even lead to death in Scrub typhus, from pneumonia, heart disease, internal bleeding, meningitis or encephalitis, and multi-organ failure. Sudden onset of fever (>104 F), rashes (approximately seen after seven days of fever), headache, sweating, red eyes, a black eschar (scab) and lymphadenopathy are some of the common symptoms that can be seen between 10 to 12 days of infection.
Caching it early
Complications can be averted if Scrub typhus is identified in its early treatable stages. Laboratory testing is essential to establish definitive diagnosis of Scrub typhus as its symptoms are similar to those of other infectious diseases such as typhoid fever, dengue, leptospirosis or malaria, which are also common during the monsoon. Laboratory testing for Scrub typhus is available at Sukraraj hospital. Of laboratory service is not available at some hospital, a health care provider who has previously worked in Scrub typhus endemic areas, can be consulted for proper identification and treatment. A patient is suspected if fever lasts more than five days with or without rashes (or Eschar) in a Scrub typhus endemic area.
The drug of choice for the treatment of Scrub typhus is an antibiotic called Doxycycline. Alternatively, Azithromycin is used to treat patients who are pregnant and children under eight. Currently, there is no vaccine to prevent Scrub typhus. Thus prevention is the best option. This includes wearing protective cloth, using insect repellent, not sitting or lying down on bare ground or grass and creating an environment free of rats/mice. Agricultural workers, people living in houses with bushes nearby or those who travel to high-risk areas are particularly vulnerable.
Although Scrub typhus has traditionally been seen in rural areas of Nepal, it seems to be spreading in urban areas like Kathmandu as well. Chigger mites harbor typhus bacteria, which in turn are carried by rats/mice. Thus the more the exposure to rats/mice, the higher the risk of Scrub typhus. Every day, nearly half a dozen rat/mice bite cases visit Sukraraj hospital for medical consultation, suggesting that Kathmandu is at high risk of outbreak of Scrub typhus. Once mites are infected they maintain infection throughout their life, and are able to pass it on to their eggs. Policymakers, hence, should not overlook this bacterium when preparing long-term national health plans.
Moreover, policy-makers should identify at-risk groups in urban areas and campaign against the disease accordingly. As mentioned above, agricultural workers or people living in houses with bushes nearby are at increased risk. But the scenario in urban areas is different.
Acute cases
Recently, Indian researchers revealed that Scrub typhus is responsible for “Acute Encephalitis Syndrome (AES)” in which a patient develops sudden high-grade fever with altered mental status. But we still don’t know how many patients have died of or are being affected by AES in Nepal. Common symptoms may also make health care providers confuse it with Japanese Encephalitis, which is also common in Nepal. Additional research is therefore needed to better understand relationship between Scrub typhus and AES among Nepali patients.
Last year hundreds of thousands of people reportedly contracted Scrub typhus, but mortality was low. It shows that people are becoming increasingly aware of this emerging infectious disease in rural areas, where it is common. However, general public, particularly those living in urban areas, may not know about the silent shifting of Scrub typhus from rural to urban areas.
Time has come for physicians working in urban areas to consider Scrub typhus in febrile patients with clinically compatible symptoms. Early detection and treatment can minimize hospitalization and even deaths.
The author is Coordinator of the Clinical Research Unit at Sukraraj Tropical and Infectious Disease Hospital, Teku, Kathmandu
You May Like This

Flood alert raised in Koshi settlements, but no imminent danger
KATHMANDU, July 15: The Flood Forecasting Section of the Department of Hydrology and Meteorology (DHM) issued a flood alert in... Read More...

Scrub typhus claimed 11 lives, 667 people infected till Nov 15: EDCD
KATHMANDU, Jan 25: A total of 667 patients were infected by Scrub typhus in 39 districts in the current fiscal year... Read More...

EDCD deploys docs to control scrub typhus
KATHMANDU, Aug 13: Epidemiology and Disease Control Division (EDCD) of the Department of Health Services (DoHS) said that it has... Read More...





Just In
- First meeting of Nepal-China aid projects concludes
- Lungeli appointed as Minister for Labor and Transport in Madhesh province govt
- Bus knocks down a pilgrim to death in Chitwan
- One killed in tractor-hit
- Karnali Chief Minister Kandel to seek vote of confidence today
- Chain for Change organizes ‘Project Wings to Dreams’ orientation event for inclusive education
- Gold price decreases by Rs 200 per tola today
- National Development Council meeting underway











Leave A Comment